Silent danger in the veins: Understanding and preventing venous thrombosis
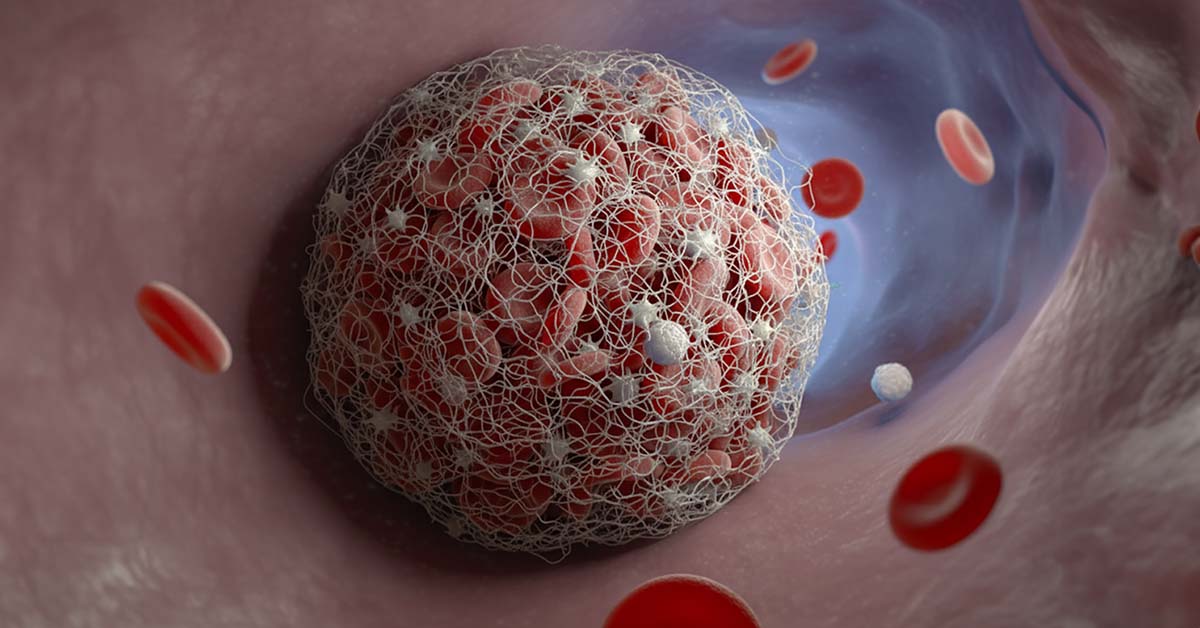
Venous thrombosis - especially deep vein thrombosis (DVT) - is a serious, often underestimated vascular disease in which a blood clot (thrombus) forms in a vein and partially or completely blocks the blood flow.
These clots most frequently occur in the deep veins of the leg or pelvis (hence the term leg vein thrombosis or phlebothrombosis).
Every year, around one in 1000 adults in Germany suffers a DVT for the first time, making it one of the most common acute cardiovascular diseases - in third place after heart attacks and strokes.
Medically tested by:
Dr. Hamidreza Mahoozi, FEBTS, FCCP
First publication:
September 18, 2025
Updated:
August 25, 2025
The main danger is that parts of the clot can break off and travel with the bloodstream towards the lungs. Such a pulmonary embolism can be life-threatening and is estimated to be responsible for up to 100,000 deaths per year in Germany. To avoid such serious consequences, it is crucial to recognize a venous thrombosis at an early stage and treat it immediately.
But how does thrombosis develop, how can it be recognized and what can be done to prevent it? In this article, you will learn about the causes, risk factors, symptoms, diagnosis and treatment options in a clear and scientifically sound way.
We also provide tips on prevention and explain the recommendations of current guidelines in Germany, Austria, Switzerland and other countries.
The aim is to provide patients and their relatives with comprehensive information – empathetic and evidence-based – so that they can recognize the “silent danger” in the veins and actively reduce their risk of thrombosis.
What is venous thrombosis?
The term venous thrombosis refers to a vascular occlusion in a vein caused by a blood clot. In principle, thromboses can occur in all vessels (including arteries), but venous thromboses are particularly relevant for venous disorders, especially in the deep veins of the legs and pelvis.
This is referred to as deep vein thrombosis (DVT). Deep veins are well protected in the muscles and transport the deoxygenated blood back to the heart. If a thrombus forms here, it can obstruct the venous return flow and lead to blood congestion. Typically, around 90% of all DVTs occur in the leg veins, often in the deep veins of the lower leg, and can spread to the knee or pelvic veins. Arm veins are less frequently affected (e.g. after infusions or injuries).
Superficial vein thrombosis: In addition to DVT, there are also thromboses in superficial veins, e.g. in varicose veins, often accompanied by inflammation of the veins (thrombophlebitis). This superficial vein thrombosis causes similar symptoms (local redness, pain) but is less dangerous as the affected veins do not lead directly to the lungs.
However, caution is advised: Superficial thrombophlebitis can extend to the point where it joins the deep vein system. This also increases the risk of a pulmonary embolism, albeit to a lesser extent, and should therefore not be taken lightly.
As a general rule, any suspected thrombosis should be clarified quickly by a doctor to avoid complications.
Causes and risk factors
The development of venous thrombosis is classically described by the Virchow triad: 1) slowed blood flow (stasis), 2) vessel wall damage and 3) increased tendency of the blood to clot. Various triggers can influence these factors and thus promote thrombosis:
- Prolonged immobility: Lack of exercise leads to slow blood flow in the legs. Sitting for long periods (e.g. on flights or in the office) and being bedridden (e.g. after operations or during illness) significantly increase the risk of thrombosis.
The term “economy class syndrome” is often used in this context when leg vein thrombosis occurs on long-haul flights due to cramped seating. - Vascular injuries and operations: Surgical procedures, injuries or trauma to the leg area can damage the inner wall of the vessel and trigger a local coagulation cascade. Vascular inflammation or diseases such as arteriosclerosis, high blood pressure and diabetes can also attack the vein wall and thus promote thrombus formation.
- Coagulation disorders: Congenital thrombophilia (e.g. factor V Leiden mutation, protein C/S deficiency or antithrombin III deficiency) lead to excessive coagulation. In around 30% of VTE patients, for example, APC resistance (factor V Leiden) is found to be the underlying cause.
A lack of anticoagulant or clot-dissolving substances can also promote thrombosis. If such a thrombophilia exists, the risk increases significantly, especially in combination with other factors. - Increased tendency to clot due to hormones: Hormonal influences play a major role. The contraceptive pill and hormone preparations (e.g. during the menopause) increase the risk of thrombosis, especially if there are additional risks such as smoking or obesity.
Pregnant women naturally have increased blood clotting – their risk of thrombosis is around five to six times higher than that of non-pregnant women of the same age.
If other factors are added (such as lack of exercise during pregnancy due to bed rest in the event of complications), the susceptibility to DVT can increase many times over. The combination of smoking and the pill is particularly critical: if a woman over 35 smokes and takes the pill at the same time, her risk of thrombosis increases dramatically – by up to 40 times compared to a non-smoker not taking the pill. - Previous thromboses or pulmonary embolisms: Anyone who has already suffered a thrombosis (or embolism) is at increased risk of further events. The vessels are often already damaged and tend to re-occlude if no adequate prophylaxis is taken.
- Chronic diseases: Cancer (especially at an advanced stage) significantly increases the risk of thrombosis through various mechanisms (tumor cells activate the coagulation system). Severe heart failure (cardiac insufficiency) also favors venous thrombosis, as the blood flow is slowed down.
In addition, hematological diseases that make the blood more viscous (e.g. polycythemia) can lead to increased clot formation. - Other factors: Varicose vein disease (varicosis) is associated with poorer blood return and venous congestion and is also considered a risk factor. Being severely overweight (obesity) increases the pressure on the leg veins and roughly triples the risk of DVT. A lack of fluids (dehydration, e.g. in summer or when not drinking enough) makes the blood more viscous and encourages clots.
Finally, the risk of thrombosis also increases significantly with age (>60 years), as vessel walls and valves undergo degenerative changes and the tendency to clot increases with age.
As you can see, venous thrombosis does not usually come “out of the blue”. Several risk factors often work together to cause a clot to form. Many of these factors can be influenced – more on this later in the prevention section.
It is important to know your personal risk situation (e.g. before embarking on a long flight or if you choose hormonal contraception) and to weigh up with your doctor whether preventive measures are necessary.
Symptoms and warning signs
Deep vein thrombosis can cause very different symptoms – from clearly visible swelling to almost no symptoms at all. Typically, however, there are some alarm signs that should be taken seriously:
- Sudden one-sided leg swelling: The affected leg (lower leg, ankle or entire leg) often suddenly becomes thicker. The swelling can increase over the course of the day. A larger circumference is often measured compared to the opposite side.
- Pain in the calf or leg: Pulling or cramp-like pain in the calf is typical, sometimes also a feeling of pressure in the thigh. The leg may feel heavy or tense, as if it has been strained like a sore muscle. The pain is often worse when standing or walking; elevating the leg sometimes provides slight relief. Pressure on certain points (calf, sole of the foot) can be painful (so-called Meyer’s or Payr’s sign), as can bending the foot strongly (positive Homans’ sign) – however, these clinical signs are non-specific.
- Skin changes: The affected leg is often overheated and the skin appears taut, shiny and discolored. Typically, a bluish (livid) or reddish discoloration can occur, caused by the backflow of venous blood. Visible surface veins become more prominent (so-called warning veins) as the blood seeks bypass circulation. In severe cases, the leg may also be pale marbled (phlegmasia alba/coerulea with almost complete occlusion).
- Feeling of tension and heaviness: Many patients report a feeling of pressure and heaviness in the leg. It feels “bulging”, as if it is about to burst. This feeling occurs particularly after sitting for a long time or after getting up in the morning and is an important indication.
- Slight fever, feeling unwell: Some sufferers have subfebrile temperatures (around 38°C), an accelerated pulse or a general feeling of illness. These non-specific symptoms are caused by inflammatory processes on the vessel wall and the coagulation process.
Important: Not all of these signs have to be present. Sometimes typical symptoms are almost completely absent – especially in immobilized or elderly patients, a DVT can be silent.
Conversely, just one of the above symptoms on the leg – especially if it occurs acutely – should make you think of a thrombosis. Because the symptoms can be so unspecific, it is also referred to as a “silent” or “silent danger”.
In fact, every third thrombosis is only discovered as a complication, e.g. when a pulmonary embolism suddenly occurs. Don’t let it get that far: If thrombosis is suspected, seek medical advice immediately!
Diagnosis: How is a DVT diagnosed?
The diagnosis of venous thrombosis is made in several steps. First, the doctor will take a thorough medical history and carry out a clinical examination.
He will ask about your symptoms (how long has the swelling or pain been present?), risk factors (e.g. recent surgery, long journey, family history of coagulopathy) and previous thromboses.
During the physical examination, he looks for visible swelling, measures the circumference of the leg and checks for pressure pain in typical areas. Clinical signs such as a positive Homans test can also provide clues, but – as mentioned – are not conclusive.
To objectively assess the likelihood of a thrombosis, many doctors use a score such as the Wells score . Certain points are awarded (e.g. for leg oedema, tumours, recent immobilization, etc.). The higher the score, the more likely a DVT is. If there is a low or medium clinical probability, a D-dimer test is usually carried out.
Laboratory: D-dimer test
D-dimers are cleavage products that are formed when a blood clot is broken down by the body. A blood test for D-dimer can be helpful: If the value is normal (negative) and the clinical probability is low, a DVT is considered very unlikely.
In this case, a negative D-dimer test rules out a thrombosis with a high degree of certainty. Caution: An elevated D-dimer value, on the other hand, does not prove a thrombosis, it only indicates that clotting or dissolution processes are taking place somewhere in the body.
D-dimers can also be elevated in cases of inflammation, after surgery, during pregnancy or in cancer, for example. The following therefore applies: If the D-dimer is positive or there is a high clinical pre-test probability, an imaging examination must be carried out.
Imaging: Ultrasound and other procedures
The gold standard for diagnosing thrombosis is color-coded duplex ultrasonography of the leg veins. This is a special ultrasound that makes both the vascular structure and the blood flow visible in color. The doctor performs a so-called compression sonography: He presses on the vein with the ultrasound probe. A healthy vein can be completely compressed, whereas a thrombosed vein does not collapse completely as the clot inside prevents this. This allows the position and extent of the thrombus to be determined very precisely. This examination is painless, has no side effects and can be repeated as often as required.
In unclear cases or in areas that are difficult to access (e.g. pelvic veins), further imaging procedures are used: classic phlebography (X-ray contrast imaging of the vein) is rarely required nowadays, for example if ultrasound does not provide clear results. Instead, magnetic resonance venography (MRV) or CT angiography can be helpful in special situations (e.g. pelvic vein thrombosis, tumor thrombosis). If pulmonary embolism is suspected as a complication, a CT scan of the lungs (CT angiography) would be performed. However, duplex ultrasound remains the method of choice for the initial diagnosis of leg vein thrombosis – fast, safe and without radiation exposure.
Treatment: How is venous thrombosis treated?
Any confirmed venous thrombosis must be treated immediately to prevent the progression of the clot and complications such as pulmonary embolism.
The treatment of DVT essentially rests on two pillars: (1) inhibiting blood clotting (anticoagulant medication) and (2) improving venous return (compression and mobilization). Modern guidelines recommend a structured approach in phases:
- Initial phase (first 5-21 days): Anticoagulation is started immediately at full intensity to stabilize the current clot or stop further growth.
Heparin is usually used – either as low-molecular-weight heparin (NMH) injected under the skin or as intravenous unfractionated heparin.
NMH (e.g. enoxaparin, dalteparin) is often preferred nowadays as it can be dosed predictably and does not require ongoing blood coagulation monitoring (INR). In many cases, a heparin injection is initially administered daily. Alternatively, some new oral anticoagulants can be administered directly from day 1: e.g. rivaroxaban or apixaban in higher initial doses. This saves the heparin preliminary phase. - Maintenance and long-term therapy (at least 3-6 months): Once the acute phase is over, the patient is switched to oral anticoagulation, which is continued for several months.
In the past, phenprocoumon (Marcumar) or warfarin (vitamin K antagonists) were classically used here, which require close INR laboratory monitoring.
Today, the guidelines preferentially recommend the new oral anticoagulants (NOAC/DOAC) such as apixaban, rivaroxaban, dabigatran or edoxaban, because they cause serious bleeding significantly less frequently with comparable efficacy.
Studies have shown an approx. 40% lower rate of severe bleeding with DOACs compared to Marcumar . DOACs are also more user-friendly (fixed dose, hardly any monitoring). Maintenance therapy usually lasts at least 3 months, but often 6 months or longer – depending on the circumstances of the thrombosis. If, for example, the DVT was unprovoked (without a triggering event) or if there are persistent risk factors (such as cancer), longer or even permanent anticoagulation is often considered.
The German guidelines recommend indefinite anticoagulation at the full dose if the risk of recurrence is high. If the risk is moderate, prolonged secondary prophylaxis can be given at a reduced dose (e.g. half the DOAC dose) in order to reduce the risk of recurrence and minimize the risk of bleeding. These decisions are made individually with the patient and reviewed regularly. - Secondary prophylaxis & aftercare (beyond 6 months): After completion of anticoagulation (or if it continues permanently at a low dose), regular check-ups are due.
The doctor checks the condition of the veins, possible late effects and adjusts the medication if necessary. It is important to sensitize patients to risk factors for future thromboses – for example, to take prophylactic measures (e.g. heparin injections, see Prevention below) at an early stage in the event of prolonged immobilization (travel, hospital stay).
Compression and movement
In addition to anticoagulant medication, compression therapy is an essential treatment measure. External pressure on the leg accelerates venous blood flow and reduces edema. Patients with DVT should wear a graduated medical compression stocking (at least class II) on the affected leg as soon as possible. This should be put on daily, throughout the day – especially when standing up, standing or sitting.
Compression not only helps acutely against swelling, but also significantly reduces the risk of post-thrombotic syndrome (PTS) in the long term. Studies show that consistently wearing compression stockings can halve the incidence of PTS.
In addition, intermittent pneumatic compression pumps are also used in hospitals for immobilized patients, which promote venous return flow by rhythmically inflating cuffs.
In the past, strict bed rest was often prescribed for DVT for fear that movement could loosen the thrombus. However, current findings and guidelines tend to allow early mobilization with adequate anticoagulation, as movement activates the muscle pump and the thrombus tends to remain fixed in place with effective anticoagulation.
In the first few days, however, heavy physical exertion should be avoided and the leg should often be elevated to reduce the swelling.
As soon as the acute phase is over, regular exercise promotes healing: walking, light gymnastics or foot rocking improve circulation. It is important that the patient is reminded to wear compression stockings, especially when getting out of bed.
Invasive therapies (lysis, thrombectomy)
In most cases, the combination of anticoagulation and compression is sufficient to treat a thrombosis. The body’s own system largely breaks down the thrombus over time. However, there are special situations in which invasive measures are considered:
- Thrombolysis (“lysis”): Medication (so-called fibrinolytics such as rt-PA, streptokinase or urokinase) is used in an attempt to actively dissolve the clot. However, this carries a higher risk of bleeding (e.g. cerebral haemorrhage) and is therefore only used in selected cases – for example in the case of extensive thrombosis affecting the entire leg or if there is an acute risk to life due to pulmonary embolism.
Lysis therapy is also indicated for so-called phlegmasia cerulea dolens (critical circulatory disorder of the leg due to massive DVT) in order to prevent an impending amputation. Lysis is usually carried out locally via a catheter directly into the thrombus.
Important: Thrombolysis with medication is only effective within the first few days up to a maximum of ~10 days after the onset of thrombosis – later, the thrombus is organized and more difficult to dissolve. - Surgical thrombectomy: This involves surgically removing the blood clot from the vein. This method is very rarely used, only in life-threatening situations or if lysis fails. There are various techniques: Open thrombectomy opens the vein directly and removes the thrombus manually.
Alternatively, a balloon catheter can be used, which is inserted into the vein via a small incision. The balloon is inflated behind the thrombus and when it is withdrawn, it “pushes” the thrombus out of the vessel. Occasionally, a bypass is also placed around the blocked vein to divert the blood flow.
All these procedures are reserved for specialist centers and are only considered if there is a risk of serious damage without intervention (e.g. imminent loss of the limb). - Cava screen (filter): If anticoagulation is absolutely not possible (e.g. due to high risk of bleeding from recent surgery) and a large DVT is present, a vena cava filter can be temporarily inserted into the great vena cava. This catches any clot particles that may escape and prevents a pulmonary embolism.
However, the filter is removed as soon as possible and drug therapy is started, as filters themselves can cause thrombosis in the long term.
– Note: This measure is very specific and is also rarely used; it should only be used on guideline recommendation in selected cases.
In summary, treatment aims to bring the existing thrombus under control and help the body to break it down, prevent new clots and minimize secondary damage. Acute DVT treatment is followed seamlessly by longer-term secondary prophylaxis and aftercare – in this phase, the main aim is to prevent complications.
Acute complication: pulmonary embolism
The most dangerous acute complication of deep vein thrombosis is pulmonary embolism (PE). A part of the thrombus (or even the entire thrombus) detaches and is flushed into the pulmonary arteries via the heart with the venous blood flow.
There, the clot blocks a pulmonary vessel, causing an acute lack of oxygen and circulatory strain. The spectrum ranges from small, barely noticed embolisms to sudden cardiovascular arrest in the case of a fulminant embolism. Around 40-100 thousand deaths per year in Germany are caused by pulmonary embolisms – many of them as a result of unrecognized DVT.
Symptoms of a pulmonary embolism may include: sudden shortness of breath, accelerated breathing and heart rate, chest pain that is sharp and intensifies when inhaling, a feeling of anxiety, sweating and possibly a cough with bloody sputum. Paleness or bluish discoloration (cyanosis) of lips and fingernails indicate severe oxygen deficiency.
However, small embolisms can also cause atypical or mild symptoms – e.g. just a little cough and a slight feeling of pressure in the chest.
Attention: A pulmonary embolism is a medical emergency! In the event of sudden unexplained shortness of breath or severe chest pain following a thrombosis or suspected thrombosis, the emergency doctor must be called immediately. Any suspected PE requires immediate diagnostics (CT angiography) and, if necessary, lysis therapy or intensive care, as there is a danger to life within a short time.
Long-term complication: post-thrombotic syndrome
While pulmonary embolism occurs within hours to days, post-thrombotic syndrome (PTS) often only becomes apparent as a chronic consequence weeks to months after a DVT has been overcome.
The venous valves in the affected segment are often damaged or destroyed by the thrombosis. Even if the clot itself has been broken down by the body, the vein walls and valves remain scarred and leaky. Chronic venous weakness (venous insufficiency) develops in the affected leg – this is known as PTS.
Typical symptoms of post-thrombotic syndrome are Permanent swelling of the leg (especially the ankle and lower leg), which increases during the course of the day.
Feeling of heaviness and pain in the leg, especially after standing or sitting for a long time . The skin may become discolored (brownish hyperpigmentation) and harden; congestive eczema, itching or inflammation of the skin often develop. In severe cases, open lower leg ulcers (venous ulcers) develop, which heal poorly. Secondary varicose veins also develop as a result of chronic congestion.
In summary, PTS can significantly impair quality of life – heavy legs, cosmetically disturbing skin changes and chronic wounds can restrict everyday life and mobility.
Unfortunately, PTS occurs relatively frequently: Around 20-50% of patients develop at least mild PTS symptoms in the first 1-2 years after DVT, around 30% have noticeable chronic symptoms, and around 5% suffer severe PTS with ulcers.
The best “therapy” for PTS is prevention, i.e. consistent treatment of acute DVT from the outset. Studies show that early mobilization under the protection of anticoagulation and consistent compression treatment reduce the risk of PTS.
The following treatment approaches are available for patients who nevertheless develop PTS:
- Compression stockings: Wearing compression stockings (class II/III) on the affected leg consistently throughout life is the most important measure. The pressure helps to reduce swelling and support the venous pumping function.
- Movement therapy: Regular gymnastics and walking training can strengthen the muscle-venous pump. Physiotherapy with special exercises (calf pump, toe stand, cycling in a supine position) is very helpful. Standing or sitting for long periods should be avoided – it is better to walk or raise your leg in between.
- Skin care: The skin on the lower leg needs a lot of attention. Daily application of moisturizing lotions keeps it supple and prevents cracks. Ointments prescribed by a doctor (e.g. containing cortisone) can help with the onset of eczema.
- Treatment of ulcers: Open legs are treated with special wound dressings; in addition to compression, modern wound therapy is often necessary. A wound center or a doctor experienced in phlebology should be involved here. It is important to prevent infections or treat them consistently (antibiotics if necessary). In very stubborn cases, surgical measures (skin grafting, vein bypass) may also be considered.
- Medication: To relieve PTS symptoms, vein tonics (herbal vein remedies such as red vine leaves, diosmin/hesperidin) are sometimes used to improve microcirculation. The evidence is limited, but they can help subjectively in individual cases. Anti-inflammatory drugs (NSAIDs) or creams containing cortisone can reduce local inflammation and pain. In severe cases with repeated thromboses, prolonged anticoagulation may be considered to prevent new occlusions.
PTS often requires a lot of patience and disciplined cooperation from the patient. However, with the right measures, an improvement can usually be achieved and worse consequences (such as large ulcers) avoided. Seek advice from vascular specialists here if you have persistent symptoms after a thrombosis.
Prevention: How can thrombosis be prevented?
In view of the potential danger of DVT, it is worth focusing on prevention – especially if you have risk factors.
Many thromboses can be prevented by simple measures. Prevention is divided into primary prevention (avoiding the first event) and secondary prevention (avoiding recurrence in those already affected). Here are the most important recommendations:
- Movement and activity: “Sitting is the new smoking”, they say – in fact, lack of exercise is one of the main preventable risk factors. Regular physical activity keeps the venous blood flow going. Just 30 minutes of walking, cycling or swimming most days of the week significantly reduces the risk.
Small habits help in everyday life: climbing stairs more often instead of taking the elevator, getting up every hour at the office and walking a few steps, getting up every 1-2 hours on an airplane or doing calf exercises while sitting down.
Vein exercises (rocking with your feet, alternating between tiptoe and heel position) can also be performed anywhere. Important: Avoid sitting or standing for long periods – if there is no other option, take breaks as often as possible. - Aim for a normal weight: Being overweight puts a strain on the leg veins. Weight reduction reduces venous pressure and improves general vascular health.
A balanced, healthy diet – rich in vegetables, fiber, low in sugar and saturated fats – not only supports the cardiovascular system, but also helps to regulate weight. Drink enough (at least 1.5-2 liters per day of water or unsweetened tea), especially when traveling or in summer, to keep the blood “thin”. - Quit smoking: Smoking damages the blood vessels and promotes inflammatory reactions. Especially in combination with other factors (contraceptive pill, pregnancy), it increases the risk of thrombosis.
Quitting smoking is one of the most important preventive measures – it not only has a positive effect on thrombosis, but also on overall health. Quitting smoking for just a few months significantly improves vascular function. - Compression stockings in high-risk situations: If you know that you will be immobile for a longer period of time – for example a long-distance flight (>4 hours) or a bus/car journey – wear compression stockings (class I or travel stockings) as a precaution.
These exert pressure on the legs and prevent the blood from pooling in the veins. Also, stand up regularly when you are out and about, keep your feet moving and drink enough.
In the case of planned operations, doctors at the hospital pay attention to thrombosis prophylaxis: patients at risk are often given prophylactic heparin injections, as well as compression stockings or pneumatic compression. Do not hesitate to actively raise the subject with your doctor – especially if you have already had a thrombosis. Bedridden persons (e.g. those in need of care or in childbed) should also wear compression stockings and be mobilized as far as possible. - Minimize risk factors: Try to eliminate controllable risks. This includes, for example, switching to other contraceptives in consultation with your doctor if you have additional risk factors (smoking, genetic thrombophilia, severe obesity). Well-regulated blood pressure and blood sugar levels (in the case of hypertension or diabetes) also protect the blood vessels.
Varicose veins should be treated – modern, minimally invasive procedures (laser, radio waves or vein glue) can remove varicose veins and thus eliminate a potential source of thrombosis. Ultimately, it is the sum of many small lifestyle changes that, when combined, have a significant preventative effect. - After a thrombosis: Secondary prevention! Anyone who has already had a DVT (or pulmonary embolism) must be particularly vigilant. The risk of a recurrence is increased, especially in the first few years after the event. Therefore, all of the above measures apply twice as much to those affected.
The doctor will often recommend that you continue to take blood thinners (e.g. low-dose DOAC) for some time after the acute phase – take these for as long as prescribed. Check-ups (ultrasound) should be carried out as recommended by your doctor in order to detect a new thrombus in good time.
To summarize: There is much to be gained from a vein-healthy lifestyle – exercise, normal weight, stopping smoking. In addition, medical prophylactic measures such as heparin injections or compression stockings protect against thrombosis in clearly defined risk situations. Many of these preventive steps may sound trivial, but they are extremely effective. The guideline on thrombosis prophylaxis emphasizes that this can prevent a large proportion of venous thromboembolisms.
Guidelines and evidence-based recommendations
Venous thrombosis is diagnosed and treated in Europe and worldwide according to clear guidelines drawn up by experts based on the latest scientific evidence. In Germany, a comprehensive guideline on the “Diagnosis and treatment of venous thrombosis and pulmonary embolism” was last published in 2023.
It was led by 17 medical societies – including the German Society of Angiology (DGA) – and also included contributions from Austria and Switzerland.
Similar recommendations are implemented in the Netherlands, Denmark, Sweden and other Scandinavian countries, as all these guidelines are based on international studies and consensus papers.
Some important key statements of the guidelines (simplified for patients) are:
- Rapid anticoagulation: As soon as a DVT is diagnosed, anticoagulation should be started without delay – this is confirmed by all guidelines. The sooner treatment is started, the lower the risk of embolism and the better the chances of the vein recovering.
- DOACs preferred: New oral anticoagulants (DOACs) are recommended as the first choice – provided there are no contraindications – because they are as effective as vitamin K antagonists, but have fewer bleeding complications and are easier to use.
Exceptions are special situations such as severe renal insufficiency or antiphospholipid syndrome, where heparin or Markumar are still used. Heparins are also preferred in pregnancy, as DOACs are not approved here. - Treatment duration according to risk profile: The guidelines clearly define the minimum duration of anticoagulation – usually 3 months, in certain constellations 6 months. After that, depending on the risk profile, a decision is made as to whether to continue treatment. In the case of unprovoked DVT or permanent risk factors (e.g. thrombophilia, active cancer), anticoagulation tends to be continued for longer or indefinitely.
A reduced maintenance dose (e.g. rivaroxaban 10 mg daily or apixaban 2.5 mg twice daily) may be considered after the first 6 months, as studies have shown that this low dose effectively keeps the risk of recurrence low, but has fewer side effects. The individual risk-benefit assessment (risk of new thrombosis vs. bleeding risk of blood thinning) is always paramount here. - Diagnostic strategy: A staged approach is recommended for diagnosis: first assess the clinical probability (e.g. Wells score), then use D-dimer if the risk is unclear, and finally confirm with imaging (primarily duplex ultrasound). This is to avoid over- and underdiagnosis. If pulmonary embolism is suspected, a similar procedure is followed, if necessary with immediate CT if there are high-risk symptoms.
- Interdisciplinary management: The guidelines emphasize that different specialists should often work together – GPs, angiologists, phlebologists, radiologists and emergency physicians, depending on the situation.
Vascular specialists and phlebologists are particularly needed for follow-up care (prevention, treatment of PTS) to ensure the best possible care. - Patient training: Another point is patient education. Every thrombosis patient should receive instructions on everyday behavior, signs of complications (when to see a doctor) and the need for adherence (take medication regularly, wear compression stockings). Informed patients have been shown to have better outcomes as they can actively participate (keyword: lifestyle measures, see above).
For patients in Germany, Austria and Switzerland, there are also numerous information offers and flyers from vascular societies, health insurance companies (e.g. AOK) and health portals that summarize the guideline recommendations in understandable language. Use these reputable sources to find out more.
What is important is that the treatment of venous thrombosis is now carried out according to recognized standards everywhere, so that you can rely on evidence-based therapy – whether in Berlin, Vienna or Stockholm.
Vigilance and precaution save lives
A venous thrombosis is not an event that can be ignored. The risks are too great if a pulmonary embolism occurs or chronic damage remains untreated.
At the same time, however, it need not cause panic: Thanks to modern medicine, thrombosis is very treatable and, if treated quickly, there is a good chance of complete recovery . The most important points you should take away from this article are
- Recognize: Pay attention to possible warning signs in your body. One-sided leg swelling, pain or skin discoloration are alarm signals – it is better to see a doctor once more than to overlook a thrombosis. Don’t be afraid to seek medical advice even if your leg symptoms are unclear, especially if you have risk factors.
- Treat: If a thrombosis is diagnosed, strictly follow the doctor’s recommendations. Heparin injections, tablets, compression stockings – these are all proven measures that protect you from a pulmonary embolism and minimize late damage.
Take your medication regularly and do not stop treatment just because the acute symptoms subside. The full duration of treatment (usually 3-6 months) is important to prevent recurrence. - Prevent: Live as vein-friendly a life as possible. Integrate exercise into your everyday life, avoid smoking and keep your weight under control. Especially if you know that you are susceptible (family history, previous thrombosis), talk to your doctor about additional prophylaxis in special situations.
Simple remedies are often enough – for example, a precautionary heparin injection before a long flight and wearing travel stockings to be on the safe side. - Inform: Use trustworthy sources and offers such as thrombosis training courses. Knowledge provides security. The more you know about the silent danger in your veins, the better you can protect yourself against it. And in an emergency, you will know exactly what to do.
Finally, an encouraging thought: thanks to advances in medicine, venous thrombosis is now manageable. It used to be feared and often fatal, but we now have effective drugs and methods at our disposal to save patients’ lives and reduce long-term consequences.
It is crucial to act in good time – then thrombosis loses its terror. So stay alert, take precautions and don’t be afraid to seek help immediately if you suspect something is wrong. Your vein-healthy life will thank you for it!
Sources
- German Society for Phlebology and Lymphology (DGPL): Thrombosis – Venous diseases. Patient information page of the DGPL on venous thrombosis, including definition, frequency, causes, symptoms, diagnosis, therapy and prevention. (accessed on 14.09.2025)
- Pharmacy at Globus (Palmpharma): Thrombosis – risk factors, symptoms & treatment. Health guide from a pharmacy with an overview of signs and causes of thrombosis. Includes lists of risk factors (e.g. smoking, pill, pregnancy) and describes treatment options such as heparin, thrombolysis and thrombectomy. (Accessed on 14.09.2025)
- Vorsorge-Online (Information portal laboratory values/IPF): Thrombosis: Laboratory tests for blood clotting. Article on the development of thrombosis, thrombophilia and prevention. Explains, among other things, factor V Leiden (APC resistance) as a common thrombophilia and gives tips on prevention (exercise in everyday life, avoid smoking, compression stockings when traveling). (Accessed on 14.09.2025)
- IHAMZ, University of Zurich: IHAMZ Guideline – Diagnosis and treatment of deep vein thrombosis (DVT) . Current guideline (2019) of the Institute of Family Medicine Zurich, in cooperation with Swiss specialist societies. Contains evidence-based recommendations for acute and long-term therapy (e.g. DOAC preferred over VKA, duration of anticoagulation depending on risk profile, benefits of compression therapy). (Accessed on 14.09.2025)
- S2k guideline (Germany 2023): Söffker G. et al. “10 key statements on the S2k guideline Diagnostics and therapy of venous thrombosis and pulmonary embolism”, in: Medizinische Klinik – Intensivmedizin und Notfallmedizin 118(5), 2023 . Summary of the most important recommendations of the German-Austrian-Swiss guideline revised in 2023, including diagnostic algorithm (Wells score, D-dimer, imaging) and therapeutic steps (anticoagulation, risk stratification for LE). (Accessed on 14.09.2025)
- Health Portal Austria: Deep vein thrombosis (DVT, phlebothrombosis) . Austrian health portal with patient information on DVT, incl. description of symptoms in pregnant women, risk factors and reference to national treatment standards. (Accessed on 14.09.2025)


