When sweating becomes torture: Modern thoracic surgery against hyperhidrosis
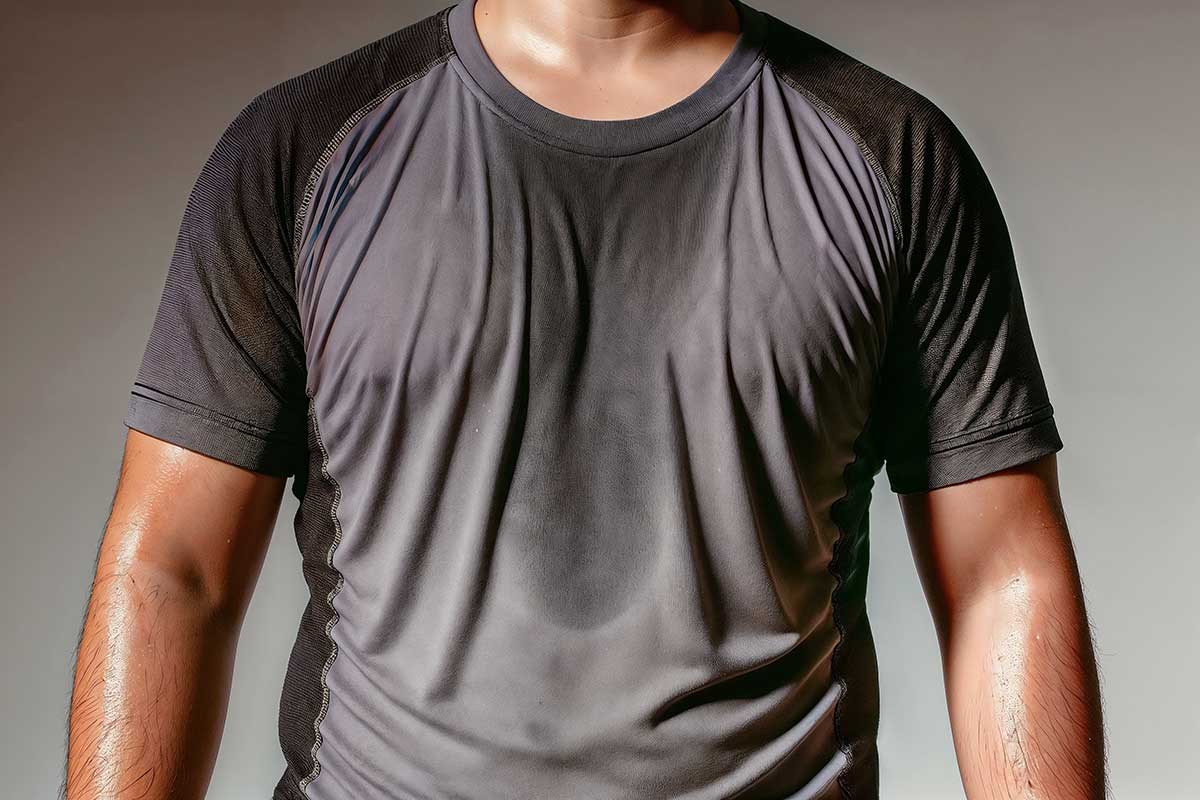
Excessive sweating - medically known as hyperhidrosis - can be a real ordeal for those affected. Constantly wet hands, soaked clothing and visible sweat stains are a burden in everyday life and often lead to great suffering.
Depending on the study, it is estimated that around 2-5% of people suffer from primary hyperhidrosis. The disorder usually begins in adolescence and affects men and women equally. Many people are not aware that there are effective therapies.
This article explains the causes and symptoms of hyperhidrosis as well as conservative and surgical treatment options.
Medically tested by:
Dr. Hamidreza Mahoozi, FEBTS, FCCP
First publication:
August 15, 2025
Updated:
August 25, 2025
The focus is on innovative thoracic sympathectomy using minimally invasive techniques – in particular uniportal VATS (video-assisted thoracoscopic surgery) without intubation, a method that can be used to stop sweating permanently.
Finally, we answer frequently asked questions and provide an outlook on how specialized centers (e.g. VenaSeal in Berlin) provide individual care for those affected.
Causes of hyperhidrosis
A distinction is made between primary (idiopathic) and secondary (symptomatic) hyperhidrosis. In primary hyperhidrosis, there is no other underlying disease – the sweat glands are actually healthy, but the control of sweat production is overactive.
The exact causes are not yet fully understood. A hypersensitivity of the sympathetic nervous system (part of the vegetative nervous system) is suspected, so that even the slightest stimuli such as stress, excitement or heat trigger an excessive sweat reaction.
Often there is also a genetic predisposition; many sufferers report familial cases. Primary hyperhidrosis typically occurs focally, i.e. it affects certain areas of the body – most commonly the palms of the hands (palmar), armpits (axillary), soles of the feet (plantar) or the face .
The first symptoms usually begin during puberty or in early adulthood.
On the other hand, there is secondary hyperhidrosis, in which the sweating is the result of another cause. Possible triggers include hormonal disorders (e.g. hyperthyroidism or menopause), metabolic diseases such as diabetes, infections, neurological diseases or certain medications.
In such cases, therapy is primarily aimed at treating the underlying disease, as the sweating is “only” a symptom.
If the sweating is generalized (all over the body), there is often a secondary cause behind it, while primary hyperhidrosis is usually localized (e.g. only hands and armpits).
Symptoms and effects in everyday life
The main symptom of hyperhidrosis is extremely heavy sweating, which goes far beyond the normal level of body cooling. Typically, those affected sweat symmetrically on the aforementioned parts of the body.
The amount of sweat can be enormous – from constantly damp, cold hands to sweat that runs off the palms of your hands in drops or shirts that are soaked through shortly after you put them on.
Many sufferers report that sweating increases even more when they are stressed, excited, in warmer weather or during physical exertion. Excessive sweating cannot be controlled voluntarily, which leads to great insecurity.
The consequences for quality of life are considerable. Social situations become a challenge: many people withdraw for fear of a “sweaty handshake” or embarrassing sweat stains.
Studies show that around 50% of patients restrict their everyday activities due to hyperhidrosis and constantly have the feeling that the condition is taking over.
Almost 70% develop chronic worry, anxiety or depression as a result of sweating. Up to 48% rate their quality of life as poor or very poor – a figure that is comparable to severe chronic skin diseases.
Heavy sweating can be just as problematic at work: Damp hands make it difficult to handle paper, instruments or electronic devices; some even choose their profession according to where sweating is the least obstructive.
The constant mental stress can trigger a vicious circle – stress increases sweating, and sweating creates new stress . Many sufferers are ashamed and reluctant to seek help, even though hyperhidrosis is treatable.
In summary, hyperhidrosis can have a massive impact on quality of life: in addition to the physical symptoms, many people suffer from social isolation, low self-esteem and emotional stress. It is therefore all the more important to know that there are effective treatments that make a normal, dry life possible again.
Conservative therapy vs. surgical treatment
Before surgery is considered, conservative treatments are the first priority. For mild to moderate hyperhidrosis, these non-surgical measures can often provide significant relief. The most important approaches include:
- Antiperspirants (aluminum chloride): Special antiperspirant deodorants, gels or solutions with aluminum chloride are usually the first choice – especially for underarm perspiration.
They temporarily block the ducts of the sweat glands, which can significantly reduce sweat production. They must be used regularly (often at night).
Disadvantages are possible skin irritation and, in the case of very heavy sweating, often insufficient effect. - Tap water iontophoresis: The hands or feet are placed in a tub of water through which a weak direct current flows.
Several sessions per week lead to a reduction in the activity of the sweat glands. Iontophoresis is a recognized therapy standard for hand and foot sweating. Many patients achieve a noticeable (albeit often only temporary) reduction in sweating.
However, the method requires a lot of discipline and time, as treatment must be carried out frequently (several times a week) at the beginning and regular applications (about once a week) are still necessary for maintenance. - Botulinum toxin injections (Botox): Botox can almost completely stop sweat production locally by blocking the transmission of stimuli to the sweat glands.
Axillary hyperhidrosis (armpits) in particular is successfully treated with Botox, but it can also help on the palms of the hands or face.
The treatment is carried out on an outpatient basis with many small injections into the affected skin region. After a few days to two weeks, sweating is significantly reduced. The effect usually lasts 4-9 months, then the procedure must be repeated.
This is feasible and effective for the armpits; the treatment is also effective on the palms of the hands, but quite painful due to the many punctures (a local anesthetic can help here). Botox is considered a proven method with high effectiveness, but is costly in the long term and limited in time. - Tablets (systemic medication): Anticholinergics are sometimes used to inhibit sweating (active ingredients such as glycopyrronium bromide or oxybutynin). These block the neurotransmitter acetylcholine in the body and can therefore reduce sweat secretion.
However, side effects often occur – including dry mouth, palpitations, visual disturbances or constipation – so that long-term use is often not tolerated.
Herbal tranquilizers (sedatives) have also been tried, as stress increases sweating; however, their effect is usually minimal. - Local surgical procedures: For severe underarm sweating, there are also procedures directly on the sweat glands in the armpit. These include sweat gland curettage or suction curettage/liposuction in the armpit area, in which sweat glands are suctioned or scraped out.
These procedures can significantly reduce the amount of sweat in the armpits and have the advantage that no nerves are severed.
However, they are only an option once the above methods have been exhausted and they only help locally in the armpit, not with sweating in the hands or other areas.
Newer devices such as microwave therapy (e.g. MiraDry) destroy the sweat glands in the armpits using heat, which can also be successful in selected cases.
Despite these various conservative options, a permanent cure for primary hyperhidrosis remains difficult. Many measures only have a temporary or incomplete effect.
In severe cases, when a patient suffers from persistently severe, therapy-resistant sweating and is severely restricted in their quality of life, the last option is surgical intervention: thoracoscopic sympathectomy.
This decision is only made after all conservative options have been exhausted, as even the most modern surgery is an invasive step with potential side effects.
Below we take a detailed look at this surgical treatment for hyperhidrosis.
Procedure of the operation: Thoracic sympathectomy (ETS)
Thoracic sympathectomy – also known as endoscopic thoracic sympathectomy (ETS) – is currently the only method of permanently curing primary focal hyperhidrosis.
This involves cutting or blocking part of the sympathetic nerve in the chest, which over-supplies the overactive sweat glands. This interrupts the excessive nerve impulses to the sweat glands and the affected areas (e.g. hands or armpits) remain permanently dry.
What happens during the procedure? The sympathetic border cord (main nerve cord of the sympathetic nervous system) runs in the chest on both sides along the spinal column and contains several nerve nodes (ganglia). From there, the nerve fibers run to the sweat glands in the various regions (face, hands, armpits, etc.). Depending on the area affected, the nerve must be interrupted at a certain level.
Sweaty hands (palmar) typically occur at the level of the 3rd thoracic ganglion (T3) intervened, in case of heavy underarm sweating at the level of the 4th ganglion (T4) .
Often both areas are affected – then the respective nerve sites are interrupted on both sides. The nerve signal can be suppressed by electrical cauterization (electrocoagulation), cutting/removing a piece or by clipping. During clipping, a small titanium clip is placed on the nerve to block it.
Theoretically, the clip could be removed again later to reverse the effect; in practice, however, the differences between clip and severing are small, as even a severed nerve can grow back together in rare cases. A restoration of the welding function is therefore generally not to be expected.
Surgical technique: In the past, a sympathectomy required the rib cage to be opened through a large incision and the ribs to be spread apart (thoracotomy) – a very invasive procedure with a correspondingly long recovery time.
Today, treatment is practically always minimally invasive in the form of video-assisted thoracoscopic surgery (VATS). A tiny camera and fine instruments are inserted between the ribs via tiny skin incisions (approx. 5 mm).
Surgery is usually performed on both sides in one session to eliminate sweating on both halves of the body at the same time. Traditionally, two small cuts were made on each side – one for the camera tube and one for the instrument.
In modern centers, even a single-port technique (uniportal VATS) is used: Here, a single mini-access of 5-10 mm per side is sufficient, through which both camera and instruments are inserted . This “keyhole” procedure protects the tissue as much as possible.
Once the camera is in the chest cavity, the lung on the side to be operated on is allowed to collapse slightly for a short time (sounds dramatic, but is a controlled process due to ventilation or the introduction of some CO₂).
This gives the surgeon a good view of the inside of the chest. Under video control, the identified sympathetic nerve fibers are then severed or sclerosed at the target level. The lungs are then unfolded again. The same is done on the other side. The actual procedure often only takes around 20-30 minutes per side, i.e. around 1 hour in total.
In many cases, it is not even necessary to leave a drain (tube) in the chest, as there is only minimal air entry, which reabsorbs itself.
For safety reasons, however, an X-ray is taken after the operation to rule out a significant pneumothorax (accumulation of air).
If everything is normal, the patient can often go home on the same day or after just one night of monitoring if they feel well.
Thanks to minimally invasive surgery to prevent sweating, the wounds are very small; many patients have hardly any pain postoperatively – usually at most a feeling of pressure in the chest for a few days, which can be easily managed with mild painkillers.
Anesthetic procedure: Normally, a thoracoscopic sympathectomy is performed under general anesthesia with intubation, whereby ventilation is switched to one lung.
However, innovative thoracic surgeons can also perform the procedure without intubation in so-called spontaneous breathing. The patient is not given a breathing tube or deep general anesthesia, but a combination of local anesthesia and sedation (twilight sleep).
Targeted nerve blocks between the ribs are used to anesthetize the surgical area and a vagus nerve block suppresses the urge to cough.
The patient continues to breathe independently during the operation and is hardly aware of the procedure – similar to a gastroscopy under sedation.
This non-intubated technique requires a well-coordinated team of anesthesiologists and surgeons, but offers remarkable advantages for the patient, which will be discussed in the next section.
Advantages of the modern (non-intubated, uniportal) method
The combination of uniportal access and no need for intubation anesthesia makes modern sympathectomy particularly gentle. Here is an overview of the most important advantages:
- Less pain and faster recovery: Every additional incision and every traumatization of tissue causes pain. The single-port access ensures maximum protection of muscles and nerves.
Comparative studies show that patients experience significantly less postoperative pain after a uniportal sympathectomy than with the traditional two-port technique.
In a Chinese study, the average pain score in hospital was 0.8 (uniportal) vs. 1.2 (biportal) – and fewer patients required pain medication in the weeks afterwards.
Smaller wounds heal faster and leave barely visible scars, which is also cosmetically advantageous. Without the “after-effects” of general anesthesia (no prolonged fasting, no nausea), patients are also fit again much more quickly. In fact, a comparison of non-intubated vs. conventional VATS showed that recovery and hospital times are significantly shorter.
With a procedure as minimal as a sympathectomy, patients can often be discharged on the same day, as they recover quickly.
In a Swiss study, 90% of patients with non-intubated VATS were able to go home the same day, compared to only 30% under general anesthesia – a huge advantage in terms of comfort and cost. - Lower risk of anesthesia: Intubation anesthesia puts a strain on the body and entails certain risks.
For example, a sore throat, nausea and vomiting may occur after waking up, and in rare cases, lung-related problems such as a slight sagging of the lungs (atelectasis) or even pneumonia.
Non-intubated thoracoscopy largely eliminates these anesthetic side effects. Studies show that patients undergoing non-intubated surgery experience significantly less nausea, vomiting and sore throat after the operation; the risk of ventilation-related lung damage is also reduced.
By dispensing with deep general anesthesia, there is also less strain on the cardiovascular system – an advantage that particularly benefits the mostly young, healthy hyperhidrosis patients. - High success rate (permanently dry): Thoracic sympathectomy is extremely effective. Immediately after waking up from anesthesia (or sedation), the target regions are dry in practically 100% of cases.
Patients immediately feel that their hands are warm and dry – an effect that is often described as life-changing. Long-term data show success rates (complete dryness) of around 95% for palmar sweating and 75-85% for axillary sweating. The slightly lower rate for armpits is due to the fact that additional areas of perspiration can sometimes play a role here.
Overall, over 95% of patients initially report a significant improvement in their quality of life.
Recurrences (relapses with renewed sweating in the treated areas) are rare – in experienced centers only in a few percent of cases.
If sweating does occur again, a second thoracoscopy can be performed for follow-up treatment, but this is only necessary in exceptional cases. Lasting success is therefore the rule. - High security and acceptance: Despite all fears, this procedure is very safe in experienced hands. Non-intubation in itself does not increase the risk of complications – reports and studies show that spontaneous breathing does not increase the rate of incidents such as pneumothorax or circulatory problems.
The surgical team is of course required to keep an awake patient stable, but can switch to normal intubation anesthesia at any time if necessary.
Overall, patients benefit psychologically from the “gentle” anesthesia anesthesia: Many find it reassuring not to have a general anesthetic, which lowers the inhibition threshold for surgery.
Internationally, it is reported that thanks to NiVATS, more people are taking the step towards a definitive solution because the operation is perceived as less intimidating.
For clinics, sympathectomy is even ideal for establishing a NiVATS program because the patients are young and healthy and the procedure is so well tolerated.
In summary, uniportal VATS sympathectomy has established itself as state of the art.
It is just as effective and safe as conventional endoscopic procedures, but offers that little bit of extra protection for the patient.
Specialized thoracic surgeons such as Dr. Mahoozi in Berlin therefore prefer to use the single-port technique and gentle anaesthesia without intubation to enable patients to recover more quickly.
Risks and possible side effects
As with any operation, the possible risks and side effects of sympathectomy must be considered. It is important to provide comprehensive information so that the benefits and potential undesirable effects can be carefully weighed up against each other.
Overall, thoracoscopic sympathectomy is considered to be very safe with few complications if it is performed correctly. Nevertheless, the most important points should not be concealed:
- Compensatory sweating: This is the most common “side effect” of sympathectomy. This is understood to mean increased sweating in other parts of the body to compensate for the region that has been switched off. Patients typically notice, for example, that their back, stomach, legs or the rest of their upper body sweat a little more than before the operation – especially when they are warm or exerting themselves.
In most cases, this compensatory sweating is mild to moderate and is hardly perceived as a nuisance by those affected, compared to the previously soaking wet hands.
Study results on occurrence vary widely (between 3% and almost 100% depending on definition and follow-up!), but realistically about 50% of those operated on develop some form of compensatory sweating.
Of these, around 5-10% of patients report that the increased sweating in other areas is unpleasant for them and disrupts their everyday life.
However, severe compensatory sweating, which is so pronounced that the patient regrets the operation, is rare . In most cases, the relief of dry hands clearly prevails. It is also often the case that the compensatory sweating subsides after a few months to years.
Unfortunately, there is no reliable method of predicting in advance who will be affected and to what extent. According to studies, the type and level of transection (e.g. at level T2 vs. T3, clip vs. cut) also have no clear influence on the risk.
However, this topic must be discussed in detail before the operation so that the patient can make an informed decision. - Horner’s syndrome: This is a very rare complication that occurs when the uppermost nerve ganglion (stellate ganglion, at the level of T1) is injured.
Horner’s syndrome is characterized by a slightly drooping upper eyelid, a constricted pupil and a sunken eye on the affected side.
The probability of this is extremely low (less than approx. 1 % ), as no incision is made above the stellate ganglion during a correctly performed sympathectomy.
If it does happen, the symptoms often partially or completely disappear within weeks. - Intercostal neuralgia (nerve pain): Any thoracic surgery requires access between the ribs, which can irritate the intercostal nerves that run there.
However, postoperative pain in the rib area is usually minor and subsides within a few days.
In rare cases, persistent neuralgia may occur. Studies report chronic nerve pain after sympathectomy in only a few percent of cases (less than 2-3%).
These can usually be treated well with painkillers and become less severe or disappear completely over time. - Pneumothorax (accumulation of air in the chest): During any procedure on the lungs, there is the possibility of minimal air entering the pleural cavity or a small leak in the lung.
After a sympathectomy, X-rays sometimes show a small pneumothorax, especially if the lung has not fully unfolded or tiny injuries have occurred on the surface of the lung.
In over 95% of cases, this is so small that no drainage is required. If a larger pneumothorax does occur (which is very rare), a drainage tube is inserted and the hospital stay is extended by 1-2 days.
Serious lung injuries are extremely unlikely given the anatomical position of the borderline cord and have practically not been observed in experienced hands. - Bleeding and injury to organs: Only small blood vessels run in the surgical area of the sympathectomy; relevant bleeding is therefore very rare.
In experienced hands, severe bleeding or injuries to the lungs/heart hardly ever occur. Overall, the general complication rate in larger study series is only ~1-3% (including all minor incidents).
In summary, endoscopic sympathectomy – when performed by an experienced thoracic surgeon – is a very safe operation with a low complication rate.
The most common consequence remains compensatory sweating, which you need to be aware of.
However, most patients do not regret the procedure, but would have it performed again in retrospect, as the benefits (e.g. dry hands and new self-confidence) clearly outweigh the disadvantages. The key is to have realistic expectations in advance.
A detailed consultation with experienced specialists – for example in hyperhidrosis centers – helps to weigh up the benefits and risks individually and make the right decision.
Study situation and scientific findings
The effectiveness of thoracic sympathectomy for hyperhidrosis is scientifically well documented. Numerous studies worldwide have examined the results and technical developments of this operation. A look at some important findings:
- As early as 2003, a large US study showed a prevalence of primary hyperhidrosis of around 2.8 % in the population – more recent studies suggest even higher rates (e.g. 4.8 % in the USA, 5.5 % in Sweden).
These figures underline the fact that hyperhidrosis is not an extreme rarity and that research into effective therapies is important. - In a Chinese comparative study (Chen et al., 2009) with 45 patients, the classic biportal VATS sympathectomy was tested for the first time against the newer uniportal technique.
The results in both groups showed 100% immediately dry hands without serious complications.
However, the one-port method performed better in some respects: the patients in the uniportal group had significantly less pain (average pain score 0.8 vs. 1.2) and the operation time was shorter (on average ~39 minutes vs. ~50 minutes with the two-port technique).
There was no difference in hospitalization, satisfaction and rate of compensatory sweating. The authors concluded that both procedures are effective, safe and minimally invasive, but that the uniportal technique causes less postoperative pain and therefore represents a sensible further development. - An Italian study (Elia et al., 2005) provided pioneering work for the anesthesia procedure used today. There, more than 30 patients were sympathectomized on both sides in an awake state (without intubation) in one session.
The result: No serious incidents, only a small pneumothorax occurred in approx. 20 % (<30 % lung collapse), but this did not require any treatment. The long-term results – including quality of life – were equivalent to the general anesthesia group, with even higher patient satisfaction and less effort.
These early data have made a decisive contribution to substantiating the feasibility and safety of the NiVATS method. - A NiVATS program was established in Switzerland in 2019 (Caviezel et al., 2019, published in Swiss Medical Weekly).
Here it became clear once again that NiVATS favors outpatient surgery: As mentioned, ~90% of patients were able to go home the same day, while far fewer were able to do so on an outpatient basis under conventional anesthesia .
The Swiss experience also confirmed that there were no increased complications and that the procedure is easily reproducible. - A comprehensive review article from 2021 (Hässig & Caviezel) summarized the then current literature on NiVATS sympathectomy.
The authors identified 7 relevant studies (2 of which were randomized) and concluded that non-intubated VATS sympathectomy for hyperhidrosis is safe and feasible, especially since most patients are young and healthy.
The procedure is ideally suited to being introduced in hospitals, as it has a short learning curve and can challenge and encourage the entire staff (surgeons and anesthetists).
With regard to specific advantages over the intubation method, the data is still limited (e.g. many studies with small numbers of cases), but trends show shorter recovery times, fewer side effects and the possibility of outpatient procedures. Overall, NiVATS contributes to more patients considering surgery because the range of procedures is perceived to be less risky. - Thoracoscopic sympathectomy is also recognized as a fixed treatment option in Germany. The medical guidelines (including the Dermatology Guideline on Hyperhidrosis, 2023) mention endoscopic sympathectomy as a treatment component for severe, focal hyperhidrosis when conservative therapies fail .
As a rule, health insurance companies cover the costs of a sympathectomy if pathological sweating is present and unsuccessful conservative treatment attempts have been documented.
This underlines the fact that the intervention is regarded as established and sensible.
In summary, numerous studies support the use of thoracic sympathectomy and its modern variants. The operation is very likely to result in dry hands/shoulders and sustainably improves the patient’s quality of life.
Technical innovations – such as uniportal access and non-intubation anesthesia – have been successfully tested and further developed so that the procedure is now gentler and often possible on an outpatient basis. For those affected, this means: the chance of a permanent solution to their sweating with minimal stress.
Frequently asked questions (FAQ)
What exactly does “hyperhidrosis” mean?
Hyperhidrosis means excessive sweating. The body therefore produces far more sweat than is actually necessary to regulate temperature.
This typically occurs in certain areas (palms, armpits, feet, face) and often begins in adolescence. Hyperhidrosis is a recognized medical condition – not a “figment of the imagination” – which can be very distressing for those affected.
What are the causes of excessive sweating?
In most cases, the hyperhidrosis is primary and there is no underlying disease. The autonomic nervous system – especially the sympathetic nervous system – is probably overactive and “overrides” the sweat glands. Genetics and stress often also play a role.
More rarely, sweating is caused by something else (this is called secondary hyperhidrosis), e.g. hormonal disorders (thyroid), diabetes, infections or side effects of medication . Your doctor will clarify this by taking a medical history and, if necessary, carrying out examinations before a therapy is planned.
What non-surgical treatments are available?
The first step is to try simple measures. Special antiperspirant deodorants with aluminum chloride are often recommended, which you apply in the evening – these can help with underarm sweating in particular by constricting and blocking the outlets of the sweat glands.
Iontophoresis (weak current in water baths) is often effective for sweating hands and feet. Botox injections can also “paralyze” the sweat glands locally (effective for approx. 6 months).
In addition, there are tablets (anticholinergics) that are supposed to dry out the whole body – but these can only be used to a limited extent due to side effects.
Home remedies and relaxation techniques are also tried, but can only have a slight influence at most.
Important to know: These methods can reduce sweating, but in some cases they have to be used repeatedly and often reach their limits with very heavy sweating.
When should surgery be considered?
Only when all conservative therapies have been exhausted and there is still a high level of suffering. In practice, this means that if you have tried various antiperspirants, medication, Botox etc. over a long period of time without sufficient success and your sweating continues to severely affect your professional and private life, a sympathectomy may be a sensible last step.
Of course, the possible side effects (e.g. compensatory sweating) must be weighed against the expected benefits. In certain cases – for example in the case of professionals who absolutely need dry hands (e.g. surgeons, electricians) – an earlier operation may be indicated, as sweating has serious consequences here.
An individual consultation with an experienced thoracic surgeon is important to determine the right time and the personal risk-benefit profile.
How exactly does the sympathectomy work?
This is a minimally invasive procedure on the chest. Under general anesthesia (or in certain cases under sedation, see next question), a camera is inserted between the ribs through a tiny incision and a fine instrument is inserted.
The surgeon cuts the corresponding nerve node of the sympathetic nervous system, which controls sweating, e.g. in the hand – this is done under visualization on a monitor.
Then do the same on the other side. The operation only takes about 1 hour in total. You wake up and immediately notice that your hands/armpits are dry. In most cases, no drainage is required.
After a short monitoring period, you can either go home the same day or stay overnight for safety reasons, depending on the clinic.
Is it true that the operation can be performed without general anesthesia?
Yes, in specialized centers (e.g. at VenaSeal in Berlin) sympathectomy is also performed without intubation. You are then given a twilight sleep and local anesthetic.
You are not fully conscious during the operation, but also not under deep anesthesia – comparable to a gastroscopy under sedation.
This procedure (non-intubated VATS) does not require a breathing tube and avoids many of the side effects of anesthesia. Not every patient is suitable for this (e.g. severe anxiety disorder or certain lung diseases tend to speak against it), but it usually works very well for young, otherwise healthy people.
Your thoracic surgeon and anesthesiologist can assess whether this option is suitable for you.
How long do I have to stay in hospital?
In many cases, sympathectomy is now an outpatient procedure. This means that you can go home in the evening on the day of the operation, provided that there are no complications.
Otherwise you usually only stay one night for observation and are discharged the next morning. Check-ups (X-rays) are important to ensure that there is no pneumothorax requiring treatment.
If everything is in order and you feel well, nothing stands in the way of a quick discharge.
How quickly will I be fit again?
Surprisingly quickly: most patients experience hardly any pain due to the small incisions – often only a slight feeling of pressure in the chest for a few days.
Ordinary painkillers are sufficient to relieve any wound pain. As a rule, normal everyday activities can be resumed after a few days. Heavy physical exertion or sport should be avoided for about 1-2 weeks so that everything can heal internally in peace.
Office work is often possible again after just a few days. Your doctor will give you precise instructions on this. Overall, the recovery time is very short compared to major operations.
What does compensatory sweating mean – will I get it?
This refers to the evasion of sweating to other parts of the body. If, for example, the hands can no longer sweat, the body sometimes reacts with increased sweating on the back, stomach, chest or legs in order to get rid of excess heat. Whether and to what extent this occurs varies from person to person.
Statistically, about half of those operated on get some increase in sweating elsewhere, but usually so mild that it hardly bothers them . Only a small minority (5-10%) have it to such an extent that it is perceived as a problem.
Unfortunately, it is impossible to predict who will be affected – it has nothing to do with the skill of the surgeon or your body type.
The important thing is that you are aware of this possibility. In most cases, the relief provided by the dry hands/underarms clearly outweighs the disadvantage of the somewhat heavier sweating on the torso.
Compensatory sweating can also reduce again over time. In extremely exceptional cases, you may consider removing clips (if this method was used), but these are special cases.
Your doctor will honestly discuss with you whether the operation makes sense for you and what level of risk is acceptable.
What other risks does the operation entail?
Serious complications are very rare. As with any operation, there are anesthetic risks (with general anesthesia) and minimal risks of infection or post-operative bleeding, but these are in the low single-digit percentage range.
A small air leak in the lung could cause a pneumothorax – if it is larger, a drainage tube would have to be inserted, which would extend the stay by 1-2 days.
However, this hardly ever happens because the camera access points are tiny. Injuries to important organs (heart, large vessels) are practically not to be expected in the position of the borderline cord as long as an experienced thoracic surgeon operates.
Horner’s syndrome (see above) is extremely rare at ~1 %. In short: Overall, the procedure is very safe and the risks are low. Of course, everything is done to further minimize even these small risks – e.g. through state-of-the-art imaging, monitoring devices and the routine of the surgical team.
Will the result last forever? Can the sweating come back?
As a rule, the result is permanent. The severed nerve fibers do not normally regenerate to the extent that the sweating function returns.
Long-term studies show relapse rates of 5-10% depending on the observation period, i.e. a small proportion of patients notice increased sweating in the originally treated areas again after months or years. However, this is usually much less pronounced than before the operation.
If a relevant relapse actually occurs, a repeat thoracoscopy can be performed, e.g. to cut additional nerve cords or to correct an incomplete first separation.
However, this is rarely necessary. Over 90% of patients remain permanently anhidrotic (dry) in the treated areas and are satisfied with the surgical result.
Does the health insurance company cover the costs?
Yes, as a rule yes. Endoscopic thoracic sympathectomy for primary hyperhidrosis is established as a recognized treatment in Germany and is noted in the guidelines.
Statutory and private health insurance companies therefore normally cover the costs if there is pathological sweating and conservative treatments have been tried without success.
Your doctor will document which therapies you have already had and can use this information to submit an application for cost coverage (if necessary). The clinics carrying out the treatment often take care of the approval themselves.
If in doubt, check in advance with your health insurance fund whether approval is required – in most cases, however, there are no problems.
Conclusion: Stop persistent sweating – there is help!
When sweating becomes torture, nobody has to lose hope. Primary hyperhidrosis may be an agonizing and persistent condition, but it can be permanently controlled with modern treatment methods.
Gentle measures such as special deodorants, iontophoresis or Botox always come first. But if all this is not enough and life continues to be dictated by sweating, thoracic sympathectomy offers a definitive solution.
Thanks to minimally invasive techniques – preferably as uniportal VATS – and innovative methods such as non-intubated thoracoscopy, this procedure can now be performed extremely gently, often on an outpatient basis and with a high success rate.
In most cases, patients’ hands, armpits or feet remain dry for the rest of their lives.
Of course, every operation must be carefully considered. Sympathectomy specifically destroys part of the nervous system in order to stop excessive sweating – a step that should be well explained and only carried out by experienced thoracic surgeons.
Side effects such as compensatory sweating are possible, but remain within tolerable limits in the vast majority of patients. The overall complication rates are very low.
Almost all patients report afterwards that they do not regret the operation, but above all enjoy the newfound dry feeling and self-confidence.
It is important to consult a specialist. In specialized facilities – such as the VenaSeal hyperhidrosis center in Berlin – sympathectomy is offered in the most modern form: minimally invasive, uniportal and, in suitable patients, even without intubation.
Our team has many years of experience with this minimally invasive surgery against sweating, places great value on individual care and achieves the lowest complication rates thanks to a high level of expertise.
Call-to-action: Do not hesitate to seek professional help. You don’t have to put up with constant sweating. Let our specialist thoracic surgeons advise you on whether a sympathectomy or another hyperhidrosis treatment is suitable for you.
Please feel free to make an appointment during our consultation hours – we will make time for your concerns. Together we will find the best way to escape the vicious circle of sweat and shame. For a dry, self-confident life without hyperhidrosis!
Sources
- Cesur E.E. et al. (2018). Non-Intubated Bilateral Single Port Endoscopic Thoracic Sympathectomy. Southern Clinics of Istanbul Eurasia 29(1):49-52. DOI: 10.14744/scie.2018.02986
- German Dermatological Society (2005). Hyperhidrosis – causes and current treatment options. Guideline/review paper, JDDG (Journal of German Dermatologists).
- International Hyperhidrosis Society – News Blog (2021). New Research Documents Quality-of-Life Burden of Hyperhidrosis. (Statistics on the impact of hyperhidrosis on quality of life) .
- Caviezel C. et al. (2019). Establishing a non-intubated thoracoscopic surgery program for bilateral uniportal sympathectomy. Swiss Med Wkly 149:w20064. DOI: 10.4414/smw.2019.20064
- Hässig G., Caviezel C. (2021). NiVATS sympathectomy for hyperhidrosis: should I stay or should I go? A Narrative Review. Video-assist. Thorac. Surg. 6:29. DOI: 10.21037/vats-21-11
- Chen Y.B. et al. (2009). Uniportal versus biportal video-assisted thoracoscopic sympathectomy for palmar hyperhidrosis. Chinese Medical Journal 122(13):1525-1528 .
- Elia S. et al. (2005). Awake one-stage bilateral thoracoscopic sympathectomy for palmar hyperhidrosis: a safe outpatient procedure. Eur J Cardiothorac Surg 28(2):312-317 . DOI: 10.1016/j.ejcts.2005.03.046
- University Medical Center Freiburg, Thoracic Surgery (2023). Patient information Hyperhidrosis & thoracoscopic sympathectomy. (Retrieval: 2025)
- Klinikverbund Bielefeld – EvKB Thoracic Surgery (2021). Non-intubated VATS in Bethel – Information flyer on thoracic surgery guided awake. (Retrieval: 2025)
- Children’s Hospital of Philadelphia (CHOP) (2020). Hyperhidrosis Surgery (Thoracoscopic Sympathectomy) – Patient Story. (Experience report of an adolescent patient after ETS)
- Strutton D.R. et al. (2004). US prevalence of hyperhidrosis and impact on individuals with hyperhidrosis: Results from a national survey. Journal of the American Academy of Dermatology 51(2):241-248. DOI: 10.1016/j.jaad.2003.12.040
- Doolittle J. et al. (2016). Hyperhidrosis: an update on prevalence and severity in the United States. Archives of Dermatological Research 308(10):743-749. DOI: 10.1007/s00403-016-1697-9 (prevalence ~4.8 % in the USA)
- Solish N. et al. (2008). Perspectives on the Management of Hyperhidrosis. Journal of Cutaneous Medicine and Surgery 12(5):233-244. DOI: 10.2310/7750.2008.07068 (Treatment algorithm for primary hyperhidrosis)
- Hornberger J. et al. (2004). Recognition, diagnosis, and treatment of primary focal hyperhidrosis. Journal of the American Academy of Dermatology 51(2):274-286. DOI: 10.1016/j.jaad.2003.12.029 (Consensus paper on hyperhidrosis therapy)
- Grabell D. et al. (2018). Medical Student’s Disease: addressing patient delay in hyperhidrosis treatment. International Journal of Dermatology 57(11):1335-1336. DOI: 10.1111/ijd.14115 (Reasons why patients delay therapy)
- AWMF S1 guideline (2023). Definition and treatment of primary hyperhidrosis. AWMF register no. 013-059, valid until 2028 . (German guideline: Therapy levels & cost coverage)
- Stolman L.P. (1998). Treatment of hyperhidrosis. Dermatologic Clinics 16(4):863-869. DOI: 10.1016/S0733-8635(05)70050-8 (Early review article on treatment options)
- Ro K.M. et al. (2002). Clinical profile of patients with primary hyperhidrosis. The International Journal of Psychiatry in Medicine 32(4):353-360. DOI: 10.2190/3Y0V-JWD0-7YQH-RPJ0 (Family clustering and quality of life in hyperhidrosis)
- Atkins J.L. et al. (2018). The Evolving Role of Endoscopic Thoracic Sympathectomy for Hyperhidrosis. The Thoracic and Cardiovascular Surgeon 66(2):133-141. DOI: 10.1055/s-0037-1598103 (Modern developments ETS)
- Hashmonai M. et al. (2017). The Etiology of Primary Hyperhidrosis: A Systematic Review. Clinical Autonomic Research 27(6):379-383. DOI: 10.1007/s10286-017-0451-z (Etiology and pathophysiology of primary hyperhidrosis)


